Table of Contents
Introduction
Mental health is an issue that resonates with individuals across the globe, transcending borders and encompassing a spectrum of diverse experiences. Yet, the quality of care and the prevalence of mental health challenges are starkly disparate among different socio-economic and cultural groups.
This disparity is particularly pronounced in marginalized communities, which are often systematically excluded from the mainstream fabric of society. These communities, which include individuals identifying with various racial, ethnic, gender, sexual orientation, disability, and socio-economic backgrounds, face a unique set of challenges that are deeply intertwined with their daily experiences of discrimination and exclusion.
This blog is dedicated to exploring these disparities, understanding the complex systemic barriers that hinder equitable mental health care, and examining the innovative strategies that are emerging to tackle these issues. Through a nuanced exploration of the mental health landscape within marginalized communities, we aim to foster a more comprehensive and empathetic approach to mental health care, thereby contributing to the creation of a more inclusive and equitable system for all.
Section 1: Delving into the Nuances of Marginalized Communities
1.1 Defining Marginalized Communities
Marginalized communities refer to those segments of the population that are systematically denied access to opportunities and resources due to their race, ethnicity, gender identity, sexual orientation, disability, immigration status, or socio-economic class.
These communities are often characterized by a lack of political power and social capital, which in turn perpetuates their exclusion from the mainstream. The challenges faced by these communities are multifaceted and interconnected, necessitating a holistic understanding of the complexities that underpin their struggles.
1.2 The Concept of Intersectionality
Intersectionality, a term coined by Kimberlé Crenshaw, is a critical framework that acknowledges the interconnected nature of social categorizations such as race, class, and gender as they apply to a given individual or group. It posits that individuals may experience multiple forms of discrimination and oppression simultaneously,
which can intensify their mental health challenges. For instance, a Black transgender woman might face a distinct set of barriers at the intersection of racism, transphobia, and sexism, which cannot be understood through the lens of any single identity. This perspective is essential in addressing the mental health needs of marginalized communities, as it allows us to recognize the unique struggles that arise from the complex interplay of various social identities.
1.3 Historical Underpinnings of Marginalization
The historical context is crucial in understanding the mental health challenges faced by marginalized communities today. Practices such as redlining have had long-lasting impacts on the economic stability and mental health of Black communities by limiting their access to quality housing and education. Similarly, the forced assimilation of Indigenous peoples has led to intergenerational trauma, as they were stripped of their cultural practices and connections to their land. The persecution of LGBTQ+ individuals, including the stigmatization and criminalization of their identities, has also contributed to mental health disparities within these communities.


Section 2: The Multifaceted Challenges of Mental Health in Marginalized Communities
2.1 The Role of Social Determinants of Mental Health
Social determinants of health are the conditions in which people are born, grow, live, work, and age, which are shaped by the distribution of money, power, and resources at global, national, and local levels.
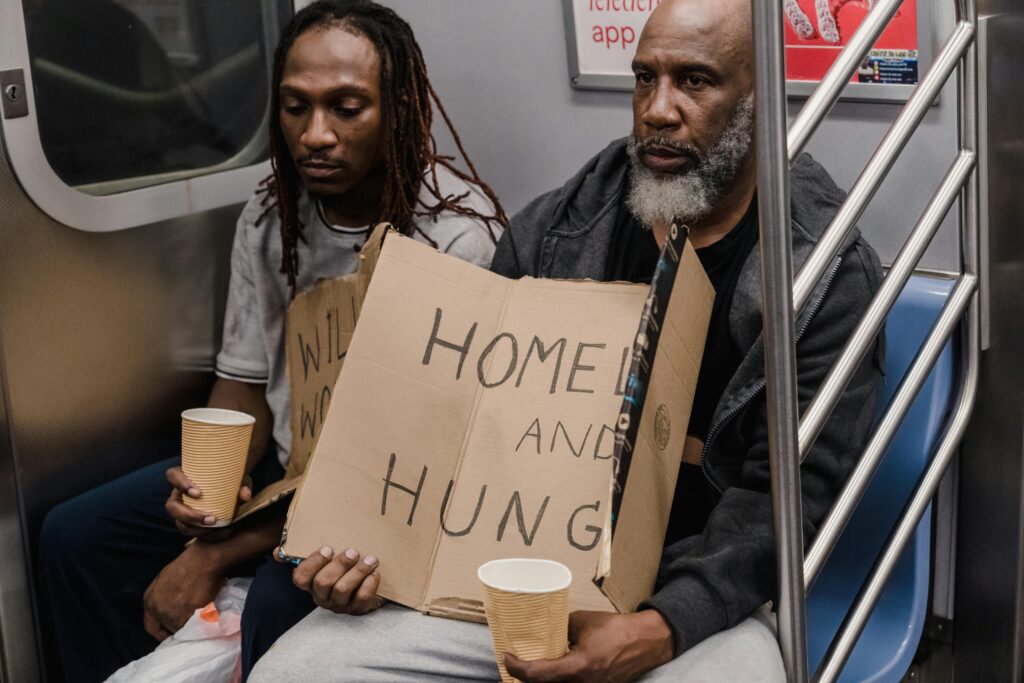
In marginalized communities, these determinants often manifest as poverty, housing insecurity, and educational disparities. These factors play a profound role in shaping mental health outcomes.
For example, individuals living in impoverished conditions are more likely to experience stress, anxiety, and depression due to the constant struggle to meet their basic needs. Moreover, living in unsafe or unstable environments can exacerbate pre-existing mental health conditions and lead to the development of new ones, such as post-traumatic stress disorder (PTSD).
2.2 The Impact of Cultural Stigma
Cultural stigma surrounding mental health can be a significant barrier to care within marginalized communities. In some immigrant groups, seeking mental health support is equated with weakness or failure to assimilate, leading to a reluctance to seek professional help. Within the LGBTQ+ community, the fear of judgment or rejection can prevent individuals from disclosing their mental health struggles to their families and communities, thereby isolating them and hindering their access to support and treatment. This stigma is often rooted in societal norms and values, which can be difficult to navigate and overcome.
2.3 Trauma and Discrimination: The Emotional Toll
Trauma and discrimination are pervasive in the lives of many marginalized individuals. Racism and discrimination contribute to chronic stress and can result in racial trauma, which is a direct consequence of experiencing or witnessing racially stressful events.
Additionally, members of these communities are disproportionately exposed to physical and sexual violence, which can have severe and long-lasting effects on their mental health. Intergenerational trauma, stemming from historical injustices like slavery and colonization, further complicates the mental health landscape, as the psychological wounds of past generations are transmitted and reverberate through the present.
Section 3: Navigating the Labyrinth of Barriers to Accessing Mental Health Care
3.1 The Financial Hurdles
The cost of mental health care is a significant barrier for marginalized communities. Despite the Affordable Care Act, which mandates mental health coverage, many individuals in these communities remain uninsured or underinsured. Even with insurance, the high co-pays and out-of-pocket expenses can deter individuals from seeking the help they need. The burden of these costs is particularly pronounced in communities already grappling with economic instability and disparities.
3.2 Geographic Inequalities in Mental Health Resources
The distribution of mental health resources is uneven across urban and rural settings. While urban areas may offer more comprehensive mental health services, these are often inaccessible to lower-income residents due to overcrowded facilities and long waiting lists. Rural communities, on the other hand, frequently suffer from a scarcity of mental health professionals, leaving residents with limited options for treatment.
3.3 Communication and Cultural Competency
Language barriers between patients and providers can lead to misunderstandings and misdiagnoses, further complicating the mental health care process for marginalized individuals. Additionally, healthcare providers may not always possess the cultural competency necessary to effectively treat patients from diverse backgrounds. This lack of understanding can result in inappropriate or ineffective treatment plans and a breakdown in the therapeutic relationship.
3.4 Historical Mistrust in Healthcare Institutions
The history of medical abuse and exploitation of marginalized communities, such as the Tuskegee syphilis study and the forced sterilization of women of color, has led to a deep-seated mistrust of healthcare institutions. This mistrust often extends to mental health care, serving as a formidable obstacle to individuals seeking help.


Section 4: Innovative Strategies to Close the Gaps in Mental Health Care
4.1 Community-Driven Solutions
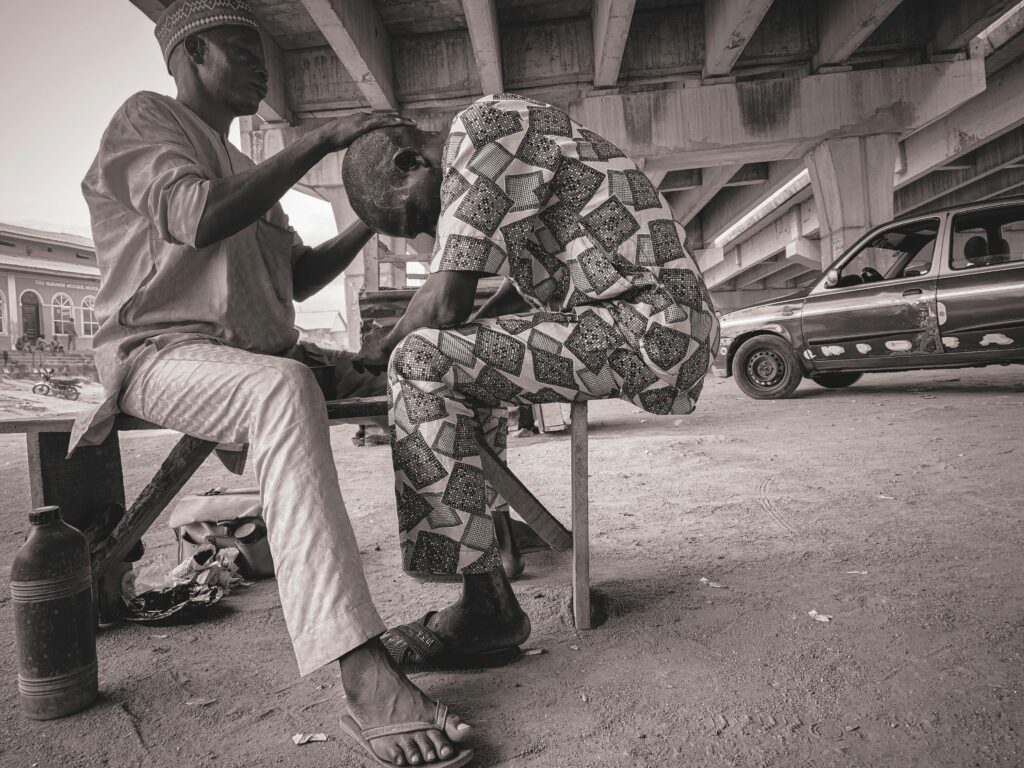
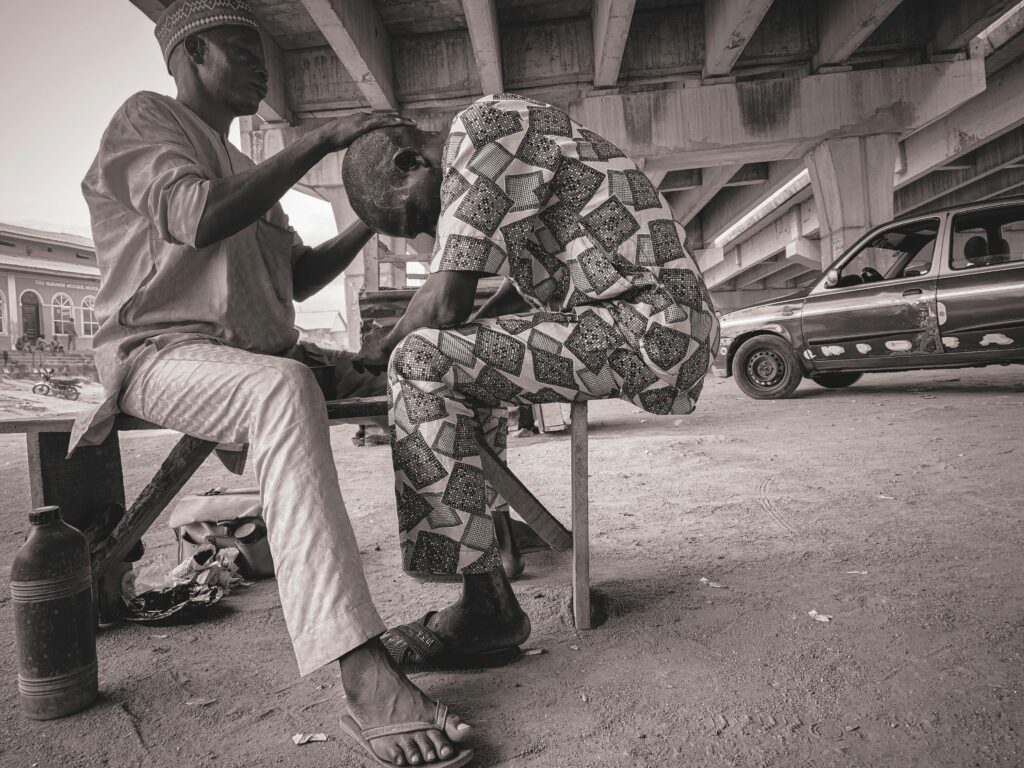
Community-based mental health programs have emerged as a promising approach to addressing the mental health needs of marginalized communities. These initiatives include community centers that provide free or low-cost counseling services and peer support networks that leverage the collective wisdom and lived experiences of individuals who share similar backgrounds. By embedding these services within communities, they become more accessible and culturally relevant.
4.2 Culturally Competent Care
Culturally competent care is essential in providing effective mental health treatment to marginalized communities. This involves training providers to recognize and understand the cultural nuances that influence an individual’s mental health and treatment preferences. It also requires the integration of traditional healing practices that resonate with patients’ cultural backgrounds, such as talking circles in Indigenous communities or yoga within South Asian groups.
4.3 Advocating for Policy Change
Advocating for policy reforms is a crucial component in the quest for equitable mental health care. This includes expanding Medicaid to cover comprehensive mental health services and supporting initiatives that aim to increase the number of mental health professionals from marginalized communities. Furthermore, enacting anti-discrimination laws and regulations can serve as a safeguard for patients’ rights and ensure that they receive the care they deserve.
Section 5: Celebrating Progress and Stories of Resilience
5.1 Successful Programs Leading the Charge
Several organizations have developed innovative and impactful programs that serve as beacons of hope for marginalized communities. The Trevor Project, for example, offers crisis intervention and suicide prevention services specifically tailored to LGBTQ+ youth, while the StrongHearts Native Helpline provides culturally appropriate support for Indigenous individuals facing domestic violence. These programs demonstrate the transformative power of community-driven initiatives that are sensitive to the unique needs of their target populations.
5.2 Personal Narratives of Triumph
Sharing personal stories of individuals who have benefited from mental health services can serve as a powerful tool in combating stigma and inspiring change.
These narratives underscore the human dimension of the issue and remind us that behind the statistics are real people with real struggles. By showcasing the successes and resilience of individuals who have navigated the mental health care system, we can encourage others to seek the help they need and foster a culture of openness and support.
Conclusion
The journey toward equitable mental health care for marginalized communities is fraught with challenges, but it is also paved with opportunities for growth and transformation.
By fostering a deeper understanding of the historical and contemporary contexts that shape these communities’ experiences, we can begin to dismantle the barriers that prevent them from accessing the care they deserve. Through community-based solutions, culturally competent care, and advocating for policy changes, we can collectively strive for a more inclusive and empathetic mental health care system.
It is our responsibility to listen to the voices of those who have been historically silenced and to stand in solidarity with them as we work toward a future where mental health is not just a privilege for the few but a right for all. Together, we can bridge the gap between the current reality and the ideal vision of a society where mental health is valued and supported across all demographics.